На 2 май 2022, д-р Игнасио Цигалини, интервенционално кардиолог и координатор на AMI кода в болница Privado de Rosario в Аржентина, извършва транскатетърна замяна на аортна клапа (TAVR) на 63-годишен мъж.
Процедурата TAVR, при която се използва катетър за фиксиране на резервен клапан върху стария, има няколко предимства пред конвенционалната хирургия, но носи повишен риск от остър инсулт. Въпреки всички предпазни мерки, пациент получава инсулт.
Точно в 13:12 ч. високоговорител в болница Privado de Rosario обявява „Код инсулт“.
Времето до лечение ще бъде рекордните 10 минути, през които ръководителят на болницата по неврология д-р Гуадалупе Мария Бруера ще вземе няколко променящи живота решения.
Инсулти в болницата спрямо инсулти, възникнали в общността
До 17% от всички инсулти се появяват по време на хоспитализация за неотложна помощ при пациенти, приети за друга диагноза или процедура, според доклад за вътреболничния исхемичен инсулт от д-р Итън Къмблър от Медицинското училище на Университета на Колорадо, публикуван в Neurohospitalist през 2015 г. Между половината и две трети от тях са периоперативни и перипроцедурни, като пациентите със сърдечна хирургия са изложени на най-голям риск.
Болничните инсулти имат значително по-лоши резултати от инсултите, започнати в общността, а не само защото се появяват при пациенти, които са по-възрастни, вече са болни и имат по-висока честота на медицински или хирургични ограничения за тромболиза. Болничните инсулти също са склонни да имат по-дълги забавяния на оценката и лечението.
Научно изявление от февруари 2022 г. от Американската сърдечна асоциация цитира доказателства, че пациентите с инсулт в болницата имат значително по-дълъг интервал от разпознаване на симптоми до невроизобразяване в сравнение с пациентите с инсулт в условията на спешно отделение (4,5 часа спрямо 1,2 часа). Проучване от регистъра Get With The Guidelines установи, че в сравнение с инсулта, възникнал в общността, времето, което е изминало от разпознаването на инсулт до тромболизата, също е по-дълго, на 81 минути спрямо 60 минути.
Причините за това включват симптоми на инсулт, които се дължат погрешно на заболяването, за което пациент е хоспитализиран, на ефекта на седация или анестезия, или на странични ефекти на лекарствата. За разлика от пациентите с инсулт, започнал в общността, жертвите на инсулт в болницата също не влизат в системата чрез спешно отделение с неговата култура на спешност. По-скоро е вероятно те да бъдат обгрижвани от персонал, който е неопитен в диагностицирането на инсулт и по-малко наясно с важността на бързите действия.
Десет ценни минути
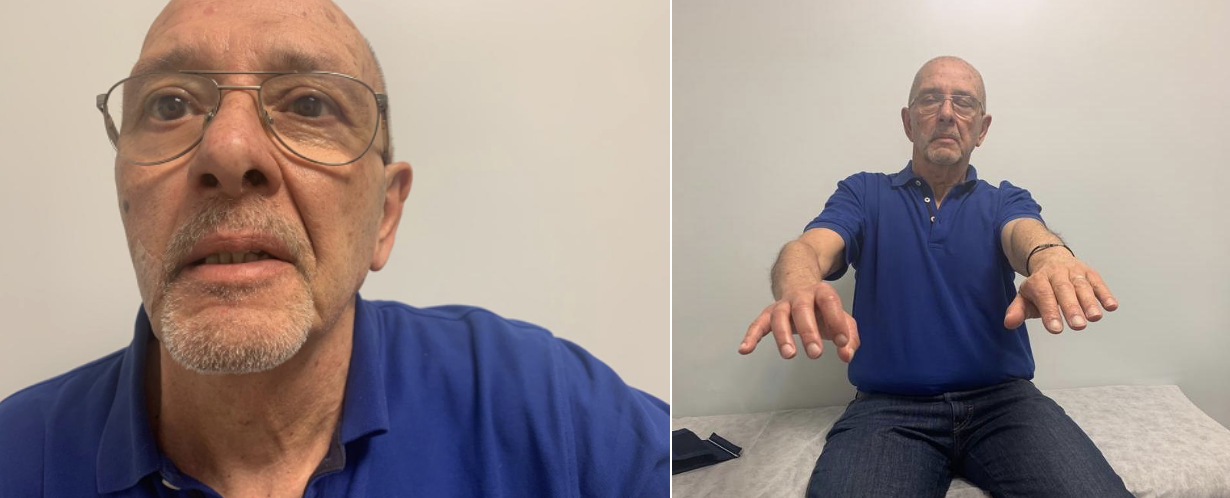
63-годишният гражданин на Росарио е един от късметлиите. Д-р Чигалини, както и всички останали в Болница Привадо де Росарио, редовно посещава обучението по кода на инсулта, което се провежда всеки месец, и е наясно с важността на незабавните действия в случай на инсулт. Когато разбира, че пациент му проявява афазия, той активира „Код инсулт“ без колебание.
На път от лабораторията за катехизисни снимки до залата за образна диагностика на кратко разстояние, оценка на NIHSS от невролога на дежурен лекар д-р Гуадалупе Брюера дава оценка от 12. С помощта на магнитно-резонансна ангиография са необходими само две минути, за да се изключи кървенето и да се локализира оклузията в сегмента от M3 до лявата средна церебрална артерия. Признавайки, че съсирекът не може да бъде достигнат с хирургична тромбектомия, д-р Брюера взема решение да тромболизира. Тя сама администрира болуса. Останалата част от инфузията ще се извърши в ОАИЛ, където пациент ще остане за 60 минути.
Д-р Цигалини е присъствал през цялото време, предоставяйки критични данни, които информират за терапевтичното решение и управлението на комуникацията със семейството на пациент.
Целият процес от активирането на кода на инсулта до лечението е отнел само 10 ценни минути.
Работата на всеки трябва да бъде уважавана
Болница Privado de Rosario приема около 219 пациенти с инсулт годишно и има средно време от вратата до иглата от 40 минути за инсулт, възникнал в общността. Средното време до лечението на инсулт в болницата е 35 минути. Обяснението се крие в ясно структуриран протокол с код за инсулт и трансдисциплинарна работа в екип, казва д-р Бруера. От решаващо значение за оптималното управление на болничния инсулт, редовното обучение с код за инсулт включва персонал от всички отделения в болницата. В резултат на това, има широко осъзнаване на необходимостта да се действа с бързина, когато се подозира инсулт, и всеки знае тренировката, когато се обяви Код инсулт.
Силно организираният път на пациент свежда до минимум забавянията на лечението, а симулациите, подпомагани от Инициатива Angels“, помагат да се определят възможностите за подобрение, но работата в екип е решаващият фактор, а сплесканата йерархия помага за мобилизирането на всички в екипа.
„Един от основните аспекти на инсулта е трансдисциплинарността“, казва д-р Брюера. „Десет до 15 медицински специалисти участват в код за инсулт, заедно със сестрински и административен персонал.
„Всеки член на този екип трябва да се чувства овластен – нещо, което не идва само от обучението, но и от примера. Въпреки че има един човек, който координира кода за инсулт, работата на всеки трябва да бъде уважавана.
„Успешният екип по инсулт е изграден на принципа, че изграждането на знания винаги е колективно. Нищо не може да се научи индивидуално.“

Основната доброта на човешките същества
Очевидно е, че 10-минутното „чудо“ на Росарио е само отчасти резултат от организацията и обучението. Успехът на този екип за инсулт също се корени в принципа, а принципите, които управляват управлението на инсулта в HPR, са неделими от личните ценности на д-р Брюера.
Тя описва себе си като „човек, който се опитва да учи ежедневно“ и своята болница като среда, която улеснява ученето: „Уча много от пациенти, медицински сестри, секретари и колеги.“
Качеството на медицината, практикувана в нейната болница, и по-специално от нейните колеги по кардиология, е една от причините тя да избере Росарио пред възможностите да изгради кариерата си другаде.
Тя казва: „Обичам страната си дълбоко, дори и с всичките й недостатъци, и по-специално град Росарио.“
Любовта към страната и ученето е семейно наследство. Д-р Бруера и братята й са отгледани от майка психолог и баща невролог, които също са учители. Тя казва: „Израснах в семейство, чиито основни ценности отразяват фундаменталната доброта на човешките същества, като подкрепа и уважение към другите.“
Тези стойности намират израз в програмата за лечение на инсулт в болница Privado de Rosario и, заедно с организирана пътека и вземане на решения за разделяне на секундата, понякога могат да направят чудо за 10 минути.





